What are the symptoms of piles?
The symptoms of haemorrhoids include:- Bright red bleeding from the anus. Blood may streak the bowel movement or the toilet paper.
- Tenderness or pain during bowel movements.
- Painful swelling or a lump near the anus.
- Anal itching.
- A mucus anal discharge.
Seek medical advice if:
- You have rectal bleeding for the first time, even if you believe you have haemorrhoids. Colon polyps, colitis, Crohn's disease, and colorectal cancer can also cause rectal bleeding. An accurate diagnosis is essential.
- You have been diagnosed with haemorrhoids, and you have rectal bleeding that is chronic (daily or weekly) or more profuse than just streaking. Though rare, excessive haemorrhoidal bleeding can cause anaemia.
How do I know if I have piles?
First, your doctor will look at the anal area. He or she will likely also insert a lubricated gloved finger and may insert an anoscope (a hollow, lighted tube for viewing the lower few inches of the rectum) or a proctoscope (which works like an anoscope, but provides a more thorough rectal examination) into the back passage.More procedures may be needed to identify internal haemorrhoids or rule out other conditions that may cause anal bleeding, such as anal fissure, colitis, Crohn's disease, and colorectal cancer.
To see further into the anal canal (into the lower, or sigmoid, colon), sigmoidoscopy may be used, or the entire colon may be viewed with colonoscopy. For both procedures, a lighted, flexible viewing tube is inserted into the rectum. A barium X-ray can show the entire colon's interior. First a barium enema is given and then X-rays are taken of the lower gastrointestinal tract.
What are the treatments for piles?
There are treatments for piles available from pharmacies or through a GP.Creams, ointments and suppositories can help relieve swelling and inflammation symptoms in the short-term. A GP may recommend corticosteroid cream for severe inflammation.
Warm (but not hot) sitz baths are a traditional therapy for piles: sit in about 8 cm of warm water for 15 minutes, several times a day, especially after a bowel movement.
Painkillers, such as paracetamol, can help relieve pain caused by piles. Products with local anaesthetic may be prescribed to treat painful haemorrhoids.
If you are constipated, a GP may recommend using a laxative.
However, these treatments do not get rid of the haemorrhoids themselves.
If you are pregnant, discuss any treatment, including dietary changes, with your doctor before proceeding.
If symptoms persist, your doctor may suggest one of the following procedures. Many can be performed as a day-case:
Injection or sclerotherapy. An internal haemorrhoid can be injected with a solution that creates a scar and closes off the haemorrhoid. The injection will only hurt a little.
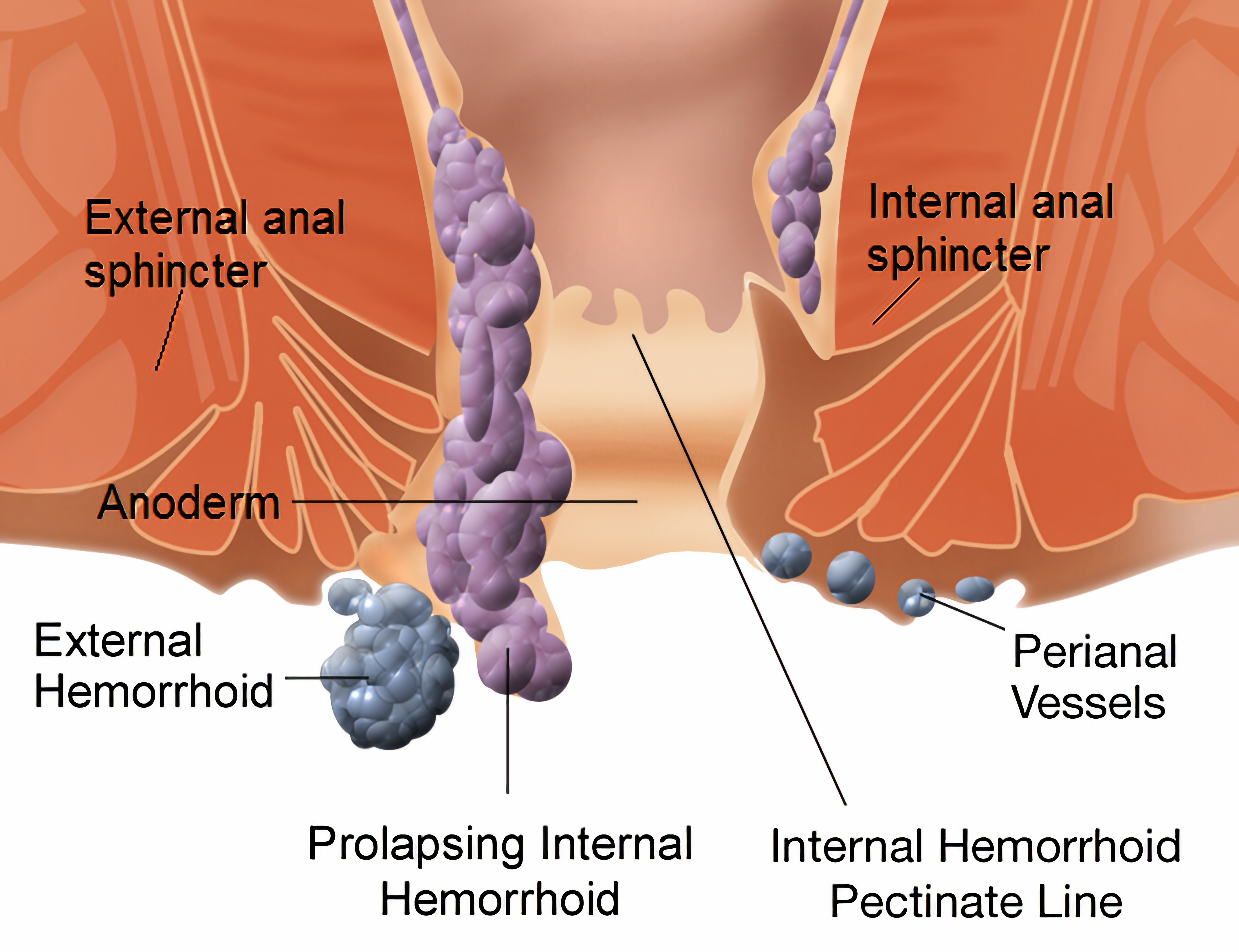
Banding. Prolapsed haemorrhoids are often removed using rubber-band ligation. A special tool secures a tiny rubber band around the haemorrhoid, shutting off its blood supply almost instantly. Within a week, the haemorrhoid shrivels and falls off.
Coagulation or cauterisation. Using either an electric probe, a laser beam, or an infrared light, a tiny burn painlessly seals the end of the haemorrhoid, causing it to close off and shrink. This is most useful for prolapsed haemorrhoids.
Surgery. For large internal haemorrhoids or extremely uncomfortable external haemorrhoids (such as thrombosed haemorrhoids that are too painful to live with), your doctor may choose traditional surgery, called haemorrhoidectomy.
The success rate for haemorrhoid removal approaches 95%, but unless dietary and lifestyle changes are made, haemorrhoids may recur.
No comments:
Post a Comment